EAR
For you to understand about the cochlear implant and how it functions, it is important that you know about the normal ear and how it functions.
The AUDITORY SYSTEM
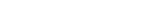
The ear consists of several parts, each with a specific function:

1-Outer Ear: the visible part, made up of the ear lobe and the ear canal.

2- Middle Ear: composed of the eardrum membrane and 3 small bones (hammer, anvil and stirrup).

3-Inner Ear:
formed by the cochlea, that contains the cells with small hairs that transform vibrations into sensory electric hearing signals (hair cells).
4- Auditory nerve: the electric impulses are transmitted to the auditory nerve, and then sent to the brain, where they will be interpreted.
The HEARING MECHANISM
The ear transforms sounds into electric signals that the brain is capable of understanding.
1) The sounds reach the OUTER EAR...
2) They pass through the EXTERNAL AUDITORY TUBE (ear canal) ...
3) And reach the EARDRUM, which vibrates.
4) The vibrations of the EARDRUM arrive at three small bones of the MIDDLE EAR (hammer, anvil and
stirrup), which vibrate and amplify the sound like a system of levers...
5) The amplified vibrations are sent to the liquid of the INNER EAR (cochlea)..
6) Following this, they reach the RECEPTOR CELLS that transform the vibrations into electric impulses.
7) These impulses pass through the AUDITORY NERVE to the brain that recognizes them as sounds.
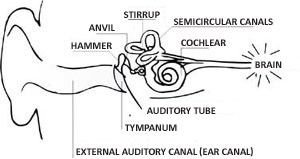
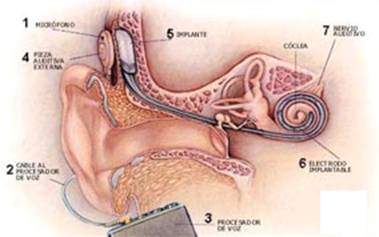
Diagram of the main structures that make up the ear.
THE Cochlear Implant
The Cochlear Implant, or more popularly known as the bionic ear, is a highly complex technological electronic device, which has been utilized in recent years to restore the function of hearing in patients with profound deafness who do not benefit from the use of conventional auditory prosthesises.
It is computerized electronic equipment that entirely replaces the ear of people who have total or almost total deafness. The implant directly stimulates the auditory nerve through small electrodes that are placed inside the cochlea and the nerve sends these signals to the brain. It is a very sophisticated device that was one of the biggest engineering feats connected to medicine. It has already existed for some years and today more than 100,000 people in the world are already using it.
What are the parts that make up the cochlear implant?
The cochlear implant is made up of two parts, an internal unit and another external.
The internal unit

Is surgically implanted inside the ear of the patient. This unit possesses a bundle of electrodes that will be positioned inside the cochlea (spiral format hearing organ). This bundle of electrodes is connected to a receiver (decoder) that is located in the region behind the ear, implanted under the skin. Together with the receiver are the antenna and the magnet that serves to fix the external unit and capture the electrical signals.
The external unit

The external unit is made up of a speech processor, a transmitter antenna and a microphone. The external unit is the part of the implant that remains visible and can be of two types: Retroauricular or type of box. The transmitter antenna has a magnet that serves to magnetically join the antenna to the internal unit (that also has a magnet).
The microphone captures the surrounding sound and transmits it to the speech processor. The speech processor selects and analyzes the sound elements, mainly the speech elements, and encodes them in electrical impulses that will be transmitted through a cable to the transmitter antenna. From the transmitter antenna the signal is transmitted through the skin by radiofrequency and arrives at the internal unit. In the internal unit we have the internal stimulatory receiver, which is under the skin. The stimulatory receiver contains a "chip" that converts the codes into electronic signals and sends the electrical impulses to the intracochlear electrodes directly stimulating the fibers of the auditory nerve. This stimulation is perceived as sound by our brain. In this way, the patient recuperates part of the hearing and can start communicating with people again.
PATIENTS WHO BENEFIT FROM THE COCHLEAR IMPLANT
The patient indicated for the cochlear implant is the one with severe to profound bilateral deafness, who was using an auditory prosthesis, but did not get a minimum satisfactory result. We divide the patients into two groups who have the symptoms and different results.
There exist patients who used to hear and for some reason have lost their hearing, who are called post-lingual patients. And there also exist patients that have been deaf since birth or lost a lot hearing even before they learnt how to speak, who are called pre-lingual patients.
Basic criteria for use of the cochlear implant :
Post-lingual patients:
Severe to profound bilateral neurossensorial auditory deficiency who will not benefit from a personal sound amplification device, or, have scores lower than 40% in sentence recognition tests with the use of the best bilateral protection possible.
There is no time limit of for the use of the cochlear implant in this group, however the greater the period of deafness, the worse the results will be.
Pre-lingual patients:
Severe to profound bilateral neurossensorial auditory deficiency with effective speech therapy rehabilitation for at least 6 months (children from 0 to 18 months) or since diagnosis (children older than 18 months), who will not benefit from a personal sound amplification device.
This age group of patients is important.
For children, the ideal age is between 1 and 5 years of age, being that the earlier the patient has the implant, the better the results will be.
From 5 years old patients can also have implants; however the results will depend on other factors such as the degree of language development already acquired and of the work of prior auditory stimulation, like the use of an auditory prosthesis and the capacity reading to read lips and sign language.
stages followed before THE IMPLANT COCLEAR
The cochlear implant is a complex process that requires the joint action of a multidisciplinary team (several professionals from different specialties) in order to achieve successful treatment.
The team consists of an Otorhinolaryngologist, a speech therapist and a psychologist (all of the team members should have a specialization with cochlear implants).
The evaluation of the candidate for the cochlear implant is a complex process and can be lengthy, therefore stages exist that are compulsory to follow and be fulfilled by all patients in order to obtain the best possible results to benefit the patient.
Medical evaluation
Initially the patient should be evaluated by the Otorhinolaryngologist to diagnose the cause, type and gravity of the deafness.
The doctor evaluates the cause that led to the deafness allowing for the cochlear implant to be inserted.
It is also important that the existence of other illnesses is studied, as the patient should be evaluated as a whole and not just the hearing
Speech Therapy evaluation
The next step is evaluation by the speech therapist, who will carry out a series of auditory and language tests, as well as exercises that will prepare the patient to receive the cochlear implant.
The evaluation of the speech therapist can be delayed and depends a lot on each case and the motivation of the patient; this evaluation is composed of:
- Evaluation of the degree of deafness: we have to be sure that the deafness is actually profound.
- Evaluation of how the patient adapts with a conventional auditory prosthesis: we have to be sure that a conventional prosthesis would not already be sufficient to attend to the needs of the patient.
- Evaluation of expressive language (speaking, use of sign language and written - in already literate patients) and receptive (effective achievement of lip reading, use of sign language and written).
When some of these aspects are met satisfactorily the patient can be sent for speech therapy rehabilitation for a determined period, and subsequently return for evaluation. In this period it will be necessary to:
- Train to read lips for adults and larger children: This training is essential in the pre-implant phase and changes the final result a lot when completed well.
- Auditory training (improving much more the performance of the patient with a conventional prosthesis or the final result with an implant).
- Therapy to stimulate language
Psychological Evaluation
It is very important that the psychological aspects of the patient are evaluated and of the people who live with them every day. It is important that the psychologist evaluates if the patient is prepared to be submitted for surgery, if they accept the fact of living with a prosthesis implanted in the head, if the family are motivated and supportive of this decision (we consider support and family participation fundamental). We also need to evaluate the degree of the patients expectations and if he is aware of the results that can be achieved. The patient has to be aware of everything that is happening and the team should explain everything in a clear and sincere way, as we believe that a relationship of mutual trust between the patient and the team is fundamental.
At the end of the pre-surgical process the patient is submitted for pre-operative evaluation so that they can be evaluated for all possible surgical risks and the surgery can happen in the safest possible way.
Examinations that are normally performed
Complete Audiometry
Audiometry in the field with use of AASI
BERA
Otoacoustic emissions
Computerized tomography and magnetic resonance.
surgical procedures
The placement of an internal unit is performed with surgery and lasts approximately 2 hours.
General anesthesia is used, or in other words the patient will be intubated and unconscious and will not feel anything during the procedure.
1) The cut (incision): The surgery is performed through the ear and a small cut in the skin of approximately 4cm.

2) Placement of the electrodes: This happens in an opening in the cochlear (auditory organ in the format of a snail) and the electrodes are inserted in the cochlear making a full circle of its interior.
3) Fixing the internal processor: The internal processor is placed below the scalp behind the ear (the patient will feel a small elevation in this area)

4) At the end of the surgery the skin is closed with stitches and a compression bandage is placed in the area.

possible risks of surgery
Primarily risks exist that exist in all surgery with general anesthesia but with the development of medicine, today it is very rare for this to happen in good hospitals.
The actual risks of the procedure are infrequent, but do exist. Below they are listed in order of frequency:
- Unsuccessful placement of the cochlear implant: this can occur if there have been anatomical changes to the patients ear, due to a congenital defect (from birth) or as a result of infections or fractures.
- Infection and necrosis of the skin: this is due to the fact the prosthesis is placed on the skin and if it occurs it can be treated if diagnosed quickly.
- Dizziness: this can occur because the organ responsible for hearing is also responsible for balance, but it is a transitory complaint that gets better quickly in a few weeks.
- Facial paralysis this is the complication most feared. This can occur because the nerve that controls the movements of the face passes very close to the area of surgery. To avoid this complication a device called a facial nerve monitor is used which reduces the risk of this complication. This complication despite being possible is very rare and generally improves after a few weeks of treatment.
- Meningitis and liquor fistula: These were complication which occurred at the start of cochlear implants. Today they are extremely rare complications.
Post-operative routine
In most cases the patient is discharged the same day as surgery.
The bandage stays on for 24 hours and the stitches are removed after 2 weeks.
The activation of the cochlear implant occurs 30 to 40 days after the procedure.
After the programming process starts and adapting the patient to the cochlear implant in consultation with a speech therapist. At the start these evaluations will be weekly and afterwards fortnightly and monthly.
post-operative care that should be taken
Do not wash the head for 3 days. After 3 days the head can be washed but care should be taken not to let water enter the operated ear, protecting it with a plug until returning to the doctor.
Sleep with the operated ear upwards for 14 days.
Do not do physical exercise or stay in the sun for 30 days.
Don't forget to take the correct medication prescribed by the doctor and don’t forget to attend the post-operative consultation.
There are no eating restrictions.
If you use an auditory prosthesis in the other ear, it can be put in as soon as the first day after surgery.
caring for your cochlear implant
The cochlear implant is prosthesis and can break if it suffers some trauma.
prohibited:
- Having a magnetic resonance examination or be close to the examination room: the implant is made of metal which can be attracted to magnetic resonance device leading to serious complications. Some models exist that allow for the examination in very special conditions, but it is obligatory to always advise the Otorhinolaryngologist and the Radiologist that a magnetic resonance examination has been requested.
- Keep the device turned off on aircraft during takeoff and landing: it functions like any electronic device and can interfere with the aircraft control equipment.
- Use of electronic bistoury: it is prohibited to use on patients with a cochlear implant, as it can burn the internal unit. Advise the doctor every time you are submitted for surgery.
Examinations that you can have without problems:
- Diagnostic Ultrasonography
- Simple radiography.
- Computerized Tomography
- Ultra violet light at orthodontic clinics.
can the function of THE COCHLEAR IMPLANT change:
- Metal detection systems: the cochlear implant will activate every time you pass through these devices (generally they are present in doors of banks and airports). Because of this, it is advisable to always carry the receipt issued by the manufacturer, proving that the patient has the implant.
- Electromagnetic radiation: Computer monitors, televisions, microwave ovens. Proximity to these devices can alter the sound quality or interfere with the transmission of data between the internal and external units.
- Store security systems: turn off the device when passing through shop doors that have an electronic security system (these are devices that beep when someone tries to leave without paying). The cochlear implant generally does not activate these devices, but sound distortion can occur and discomfort for the user of the implant.
Criteria for indicating patients
(Decree 1.278/GM of 20th October 1999)
IMPLANT IN ADULTS
The Cochlear Implant in adults should be indicated based on the following criteria:
a) people with bilateral neurossensorial profound deafness with established linguistic code (cases of post-lingual deafness or pre-lingual deafness, adequately rehabilitated);
b) absence of benefit with an auditory prosthesis (less than 30%vocal discrimination in tests with sentences);
c) psychologically suitable and motivation to use the cochlear implant.
IMPLANT IN CHILDREN
The Cochlear Implant in children less than 18 years of age with pre and post-lingual deafness should be indicated based on the following criteria:
a) experience with an auditory prosthesis for at least 3 months;
b) inability to recognize words close together;
c) family adapted and motivated to use of the cochlear implant .
d) suitable conditions for rehabilitation in the home town.
CRITERIA FOR CONTRAINDICATION
Contraindications for the Cochlear Implants are as follows:
a) pre-lingual deafness in adolescents and adults not rehabilitated by oral methodology;
b) patients with cochlear agenesis or cochlear nerve;
c) clinical contraindications.
BEnefits of the Cochlear Implant
Despite many indication criteria, not all patients benefit from the cochlear implant. Because of this the correct evaluation and orientation are fundamental for the prognostic forecast and orientation of the expectations. Many times, if the result is very limited, the implant cannot be indicated, even if the patient has profound deafness.
Studies and tracking over long periods has shown that the best results with the cochlear implant are in patients with post-lingual auditory loss and in children receiving the implant when still young (up to 2 years and 11 months) In general post-lingual individuals obtain about 80% recognition of sentences in open format; restarting professional and social activities with a significant improvement in quality of life and 50% use of the telephone without difficulties. Children who receive the implant when still babies learn oral language in an incidental way and in general, the development is very close to a normal child.
Nowadays, the benefits of the cochlear implant are already proven. Results from 877 patients studied in centers in Spain have shown gains in speech perception of around 60% in relation to pre-operative adults and 90% discrimination and speech comprehension in an open format for child with implants up to 3 years of age (Manrique etc., 2006).
In children greater than 4 years old the benefits of the cochlear implant are largely dependent on the level of development of language and perception. The better the linguistic development, the better the capacity of the child to process auditory stimuli, associating them to linguistic meaning, establishing lexical and syntactic rules of language comprehension and expression. Understanding at the appropriate level of language development, the child, despite auditory deficiency, is capable of understanding by lip-reading or LIBRAS (Brazilian Sign Language), without gaps in development. This demand is different for each age group, therefore the older the individual is, the greater language control is necessary so that he can have a better result with the cochlear implant. In a study with 54 pre-lingual deaf children with implants, aged between 4 and 12 years at the moment of activation, it takes 1 year for effective use of the implant, Guedes etc. (2005) showing that there was no significant difference between groups due to factors of sex, aetiology and age. However, children with good pre-operative language comprehension have the chance of better speech perception, 3.6 times the chance of other children (P=0.009). With this, it was concluded that pre-operative language comprehension, be it with LIBRAS and/or lip reading, is an important prognostic factor of speech perception after 1 year, and should be considered in the selection of older children for the cochlear implant.
In adolescent and adult patients with pre-lingual deafness the result depends on the expectations; there can be an excellent auditory gain even without changes to the standard of communication; the benefit is limited in the long term; and the individuals find speech perception difficult without additional means (lip reading, writing, sign language support).
BENEFITS OF THE bilateral COCHLEAR IMPLANT
For a long time bilateral hearing has been important in the localization of sound and discrimination of sentences mainly when there is more than one speaker or when there is a noisy environment.
In the same way, studies completed in pre-lingual deaf patients have shown that patients with bilateral implants demonstrate better auditory performance in these same situations. This difference in performance found in these studies although small is significant.
There still does not exist conclusive evidence in relation to small children with cognitive deafness, but based on the theory of auditory canal maturation which has its biggest development up to 2 years of age, it is believed that this group will have the greatest benefit of the bilateral implant.
This way many centers in the USA and Europe have performed bilateral surgery at the same time as the normal surgery. In Brazil, because of economic and social reason, bilateral implants are not performed, which is very reasonable when we think about the politics of public health in which we should help the greatest number of patients with the limited resources at our disposal.
A second implant was performed by this hospital on a patient who already had the implant on the other side 3 years ago. The first patient to receive a bilateral cochlear implant at this hospital was 2 years ago, however this was due to a malfunction of the first implant. This time the patient's first implant was functioning perfectly and the option of the cochlear implant was based on recent studies and the active participation of the family in this decision.
Diseases
OTITIS
Otitis Externa
It is commonly caused by humidity in the ears due to swimming in pools or at the beach, so it is much more common in the summer months. It can also be caused by excessive use of cotton buds or any other instrument put in the ear canal.
Clinical diagnosis is based on the following symptoms: ear ache and the sensation of a blocked ear, and is shown by clinical examination that the ear canal is red and swollen.
The treatment is clinical based on topical and analgesic medication and is generally resolved in a few days.
Otitis Media
Otitis Media, contrary to Otitis Externa, happens mostly in the winter months. It occurs together with the flu or a cold which affects the ear, affecting the eardrum and internal part of the ear. Because the pain is greater than Otitis Externa and the sensation of loss of hearing is also greater. It affects children more and causes greater pain mainly at night due to the cooling of the body, sometimes with high fever and general unwellness.
Diagnosis is also clinical by physical examination which shows the eardrum to be red and swollen, as well the symptoms mentioned.
Treatment is based on oral antibiotics as well as analgesics and nasal decongestants, and is also resolved in a few days.
Serous or Secretory Otitis Media
This is a complication of simple Otitis Media, previously mentioned. This occurs when there is an accumulation of secretions in the middle ear, internally of the eardrum, due to frequent bouts of flu or in children who are not breathing well, due to allergic rhinitis, enlargement of the tonsils and adenoids etc. The main symptom is loss of hearing, the child starts to become distracted and schooling is affected.
Diagnosis is clinical with a physical examination to show the presence of secretions or catarrh behind the eardrum and confirmed using Auditory and Immitanciometry examinations which demonstrate the varying degrees of hearing loss as well as a decrease in the vibration of the eardrum.
The treatment is based on oral corticoid steroids for a few days and if it has not been resolved, surgical treatment is indicated, with the placement of catheters or ventilation tubes in the eardrum to drain the secretions from the middle ear and stop them forming again, thus restoring the child’s hearing.
Perforated Eardrum
This occurs in people with a previous history of repetitive otitis, in which some of these cases of otitis perforate the eardrum which does not heal. This can also be caused by trauma, due to using cotton buds, physical aggression or abrupt pressure from waves.
The symptom is hearing reduction, as well as seeping from the ear every time the person lets water enter the ear canal. In these cases plugs are indicated for swimming or at the beach, as well as when taking a shower.
The diagnosis is clinical with physical examination in which the perforation is noted and complementary auditory examinations using Audiometry, to determine the degree of hearing loss caused by the perforation.
The treatment is surgical with a procedure called Tympanoplasty, which is microsurgery in which a graft is made to close the eardrum.
Cholesteatoma
Cholesteatoma is slightly more aggressive than otitis, in which there is growth of skin in the auditory canal inside the ear, through a perforated eardrum, causing a yellow seepage with bad odor, as well as loss of hearing to a greater degree.
The diagnosis is also clinical with a physical examination with the aid of computerized tomography which will show the extent of the disease.
The treatment is surgical with a procedure called Tympanomastoidectomy in which the eardrum is reconstructed along with a cleaning of all the skin mass which has internally attacked the eardrum.
Otosclerosis
Otosclerosis or Otospongiosis is characterized by the fixation of the bone called the stirrup, responsible for the transport of sound to the cochlear, the organ responsible for hearing inside the ear. It is more frequent in young women, having a hormonal relationship, generally occurring after pregnancy.
The main symptom is loss of hearing, possibly accompanied with buzzing or a shrill sound in the ears.
The diagnosis is done using Audiometry and eventually computerized tomography in some cases.
Deafness
Deafness or loss of hearing has various causes and levels, some of the causes have already been mentioned such as Otitis and Otosclerosis.
However other causes exist for hearing loss related to the cochlear or the auditory nerve, which have completely different treatments.
Depending on the degree of deafness, the treatment can be by using conventional hearing devices, but in many cases these are not sufficient for satisfactory hearing and actually we have various types of auditory implants that can be used for these types of deafness.
The following implants are available in Curitiba and are already part of our routine, being that a lot of health plans cover this type of surgery.
Labyrinth Diseases
These are diseases of the labyrinth and can have various causes such as changes in the spine, hearing loss, diabetes, high levels of triglycerides and cholesterol, anemia, problems in the temporomandibular (maxillary) region, among others.
The main symptoms are: vertigo, dizziness, vomiting, migraine, buzzing noises, nausea as well as other forms of unwellness.
Labyrinthitis is the commonly known name and refers to the labyrinth, which is the organ responsible for the body’s balance.
Diseases of the Labyrinth can be divided into various types according to cause to which they are related. Ménière’s disease (increase in pressure of the liquids in the internal ear canals) is one of the causes and manifests through frequent and repeated episodes of very strong vertigo, gradual hearing loss and buzzing sounds.
Dizziness is a very common symptom and is present in almost all the forms of Labyrinth Diseases. It is defined by the perception of the person’s loss of balance in relation to their surrounding environment. Vertigo is the sensation that your body is spinning or things are spinning around you.
Tinnitus also is a common symptom, occurring when the person feels that his ear is constantly producing a noise. That irritating sound can vary in volume and intensity, like the noise of a pressure cooker, shrill sounds, crickets, vibrations, etc. Some people hear so much buzzing that they cannot manage to lead a normal life, because the persistent noise can interfere with work, studying, sleep and communication with other people.
To diagnose diseases of the Labyrinth quite often a complete evaluation of the person’s health is necessary through various examinations and only when the cause has been determined can the doctor define the best treatment.